
Let’s Talk!
We’re here to help you with any questions you may have. Please don’t hesitate to reach out to us.
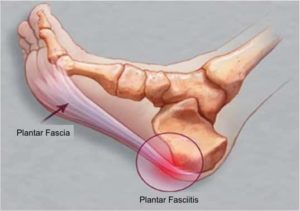
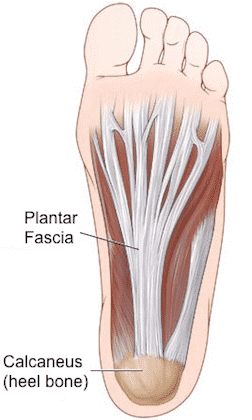
Plantar Fasciitis is a thickening of the plantar fascia which is a band in the arch of the foot. Plantar Fasciitis often causes tenderness, pain and swelling around the heel of the foot.
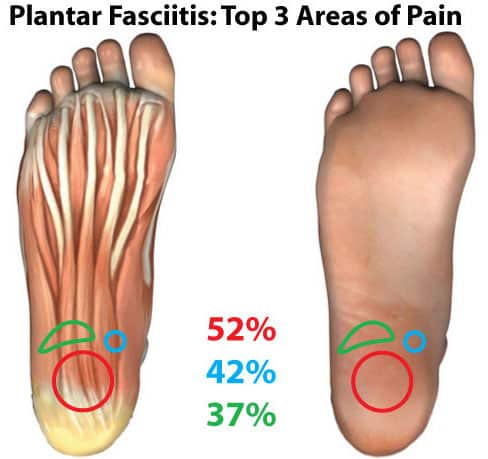
Have you ever felt pain along the inside heel of your foot? A throbbing searing or piercing pain that is just on the heel of your foot without any tingling or radiation? It might feel like your heel is walking on a stone or you have a bruising heel pain.
Has your pain gradually worsened but now is especially bad when you take your first steps in the morning and then generally fades after about 30-45 minutes?
If so, you may have Plantar Fasciitis. Sometimes it is referred to as heel-pain syndrome. It is caused by degeneration of plantar fascia as a result of persistent overuse injury. Specifically, Plantar Fasciitis is a result of micro trauma leading to degeneration and small tears of the plantar fascia. Poorly managed plantar fasciitis can significantly worsen your quality of life by interfering with your ability to do day-to-day activities.
The vast majority cases of plantar fasciitis resolve within a few months with the correct conservative management. But the longer you experience plantar fasciitis pain or delay seeking treatment, the less likely you will improve from conservative treatment.
for a more in depth discussion of Plantar Fasciitis Click Here.




Most people tend to ignore the symptoms of dull burning pain in the heel region, until it begins to affect their quality of life. For example, in some cases, individuals tend to adopt abnormal walking patterns to decrease the likelihood of acute pain attacks; however, this greatly aggravates the risk of further connective tissue damage and may lead to:
For appointments and enquires:
Phone: (774) 421-9144
This information is for educational purposes only and is NOT intended to replace the care or advice given by your physician. Always seek the advice of your physician or other qualified health provider before starting any new treatment or with any questions you may have regarding a medical condition. For more information see our Medical Disclaimer.
– Privacy Policy – Terms of Use –
Copyright 2025 © The Center for Morton’s Neuroma. All Rights Reserved.

We’re here to help you with any questions you may have. Please don’t hesitate to reach out to us.
The Center for Morton's Neuroma
